By Nancy Alexander, PT, CSCS
It’s been called the most misunderstood condition affecting women over 50. “I’m tired of being dismissed & ignored,” said a post on social media. Many are making a big deal about this mysterious hip pain women over 50 are experiencing. “It’s not arthritis, it’s menopause,” another post exclaimed. “Both my hips hurt. I think it’s tendinopathy,” said an acquaintance not too long ago. She had not yet seen a physician for this pain that was going on for about a year.
Drama aside, there is a lot of talk out there about pain located on the outside of your hips and I wanted to help you better understand all these claims. The volume of discussion alone got my attention. Turns out, there is something to all this chatter.
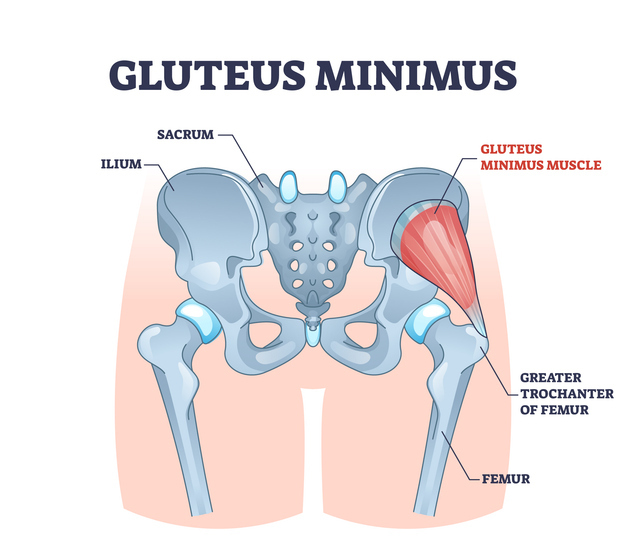
To more fully understand this condition, let’s start with some anatomy. Tendinopathy is a term used to describe a breakdown of a tendon. A tendon connects muscle to bone. There are tendons all over your body, but our focus here today is that of gluteal tendons that act on your hips. Your gluteal muscles are the muscles at your buttocks. These include the gluteus maximus, medius, and minimus. These muscles generally run from your pelvis – near where your sacrum meets your pelvis – and continue to the outer part of your hip at your side. There is a ridge at the upper part of the outside of your leg bone (femur) called your greater trochanter. The greater trochanter is where two of the three gluteal muscles attach as tendons. This is typically the site of pain with gluteal tendinopathy.

A bursa sits very close to this tendonous insertion into the femur bone. A bursa is a fluid-filled sac that helps reduce friction at the area where it is found. There are many throughout the body. This bursa often gets inflamed in concert with this condition, but realize this is a separate condition. In the past inflammation of the bursa, or trochanteric bursitis, was often used to name this condition. You may have heard of it. Now it is better understood that gluteal tendinopathy can occur on its own. This more defined diagnosis has led to better understanding and more effective treatment.
Another currently accepted name for this condition is Greater Trochanter Pain Syndrome (GTPS). A syndrome is used to describe a combination of symptoms. According to recent research, though, this syndrome is believed to be caused primarily by gluteal tendinopathy. It all comes down to the integrity of the gluteus medius and minimus tendons, especially in the aging population.
Women over 40, especially those who completed menopause, are more prone to hip pain and gluteal tendinopathy. (Physiopedia) There is your link to menopause. The condition may also affect younger people who run, ski, and dance. As many as one in three people with low back pain develop hip pain from gluteal tendinopathy. Pelvic structure and biomechanics, increased activity, and presence of hip osteoarthritis may also predispose you to increased wear and tear of your gluteal tendons near their insertion onto the femur.
An appropriate and thorough physical exam is required to differentiate your pain source and develop an effective plan of care. Imaging such as x-rays, MRI or ultrasound may help confirm the correct diagnosis.
Several conditions can affect the tendons in your hips and gluteal area, causing pain. But their underlying causes and treatments are different. Here are some of the common ones, including our topic, gluteal tendinopathy:
- Gluteal tendinitis: Repetitive movements create small micro-tears in your tendons, leading to inflammation and tendonitis. This may present with deep pain in your hip area that improves with rest, ice, compression, and elevation (RICE).
- Gluteal tendinopathy: This hip pain is the result of a tendon injury that causes tissue to break down or deteriorate. Rest doesn’t typically help, but physical therapy can ease symptoms. It takes longer to recover from tendinopathy than tendinitis.
- Trochanteric bursitis: This is inflammation in the bursa sac near these gluteal tendons at your hip. As mentioned before, these fluid-filled sacs cushion the space between bones, and tendons. Some (but not all) people with trochanteric bursitis develop greater trochanter pain syndrome (GTPS). Treatments may include nonsteroidal anti-inflammatory drugs (NSAIDs), cortisone shots, splinting, and surgery as a last resort.
(Cleveland Clinic)
Symptoms
Your health history may include potential causes of gluteal tendinopathy that include:
- Putting too much force on your tendons during physical activities (overuse).
- Tendon compression due to a fall directly onto your hip or another type of accident.
- Excess pressure on the tendons from weight gain or obesity.
- Inactivity or a sedentary lifestyle (underuse).
- Wide pelvis or hip instability.
According to the Cleveland Clinic, the most notable sign of gluteal tendinopathy is moderate to severe hip pain. This pain may extend down the outside of your leg from your hip to your knee or lower leg. You may also experience low back pain, groin pain, or gluteal (buttock) pain. This area may feel tender to touch.
The pain may feel worse when you:
- Climb stairs or walk up a hill.
- Get out of bed in the morning.
- Lie on your side. (Mostly your affected side, but pain can occur when lying on the other side, too.)
- Sit for a prolonged time or sit cross-legged.
- Stand on one leg — like when you pull on a pair of pants.
Treatment
Some research reports that about half of those suffering from gluteal tendinopathy get better on their own in up to a year. But according to the Cleveland Clinic, “7 out of 10 people with the condition see significant improvements with eight weeks of physical therapy exercises.”
If you suspect your hip pain is from gluteal tendinopathy, you can immediately take these steps to help provide relief:
- Apply heat to the painful area.
- Avoid sitting in low chairs where your hips are below your knees.
- Minimize stair climbing.
- Avoid crossing your legs, especially at your knees.
- When sleeping on your side (either side), place a pillow between your knees to help keep your top knee as high as your top hip.
- Walk on flatter surfaces (versus inclines, declines and those with side camber like a road), when possible.
Prevention
Here are some tips to help prevent gluteal tendinopathy:
- Stay physically active but pay attention to your body and signs of hip pain.
- Modify or take a break from aggravating activities that irritate your hips.
- Avoid repetitive activities that put a lot of pressure on your hips.
- Lose weight, if needed.
- Lift weights to strengthen your gluteal muscles. Bridging, roman dead lifts and dead lifts may be effective for you.
- Practice yoga or stretching exercises to keep your hip muscles flexible. Just be careful to not stretch aggressively as this may aggravate your symptoms. Your movement specialist and physical therapist can recommend a progression of stretching to address your needs.
- Treat low back pain early and practice good posture when possible. When sitting, try to position your hips slightly higher than your knees while keeping your feet flat on the floor for good support.
Summary
Moderate to severe pain from gluteal tendinopathy can affect your quality of life. It is a real thing with real solutions. Don’t let pain interfere with your ability to work, play, exercise, socialize, and otherwise have fun. Don’t let it compromise your sleep. Consult with your physician to get to the root cause of your pain and know that various treatments are available to you. Utilize the above tips to find relief fast. Physical therapy exercises can ease symptoms early and help you manage the condition over the long term. Take action now and feel better soon. Keep moving friends.
Sources:
Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/22960-gluteal-tendinopathy
Hospital for Special Surgery: https://www.hss.edu/article_gluteal-tendinopathy.asp#:~:text=Hip%20pain%20keeping%20you%20up,Casey.
Journal of Orthopaedic & Sports Physical Therapy: https://www.jospt.org/doi/10.2519/jospt.2015.5829
Physiopedia: https://www.physio-pedia.com/Gluteal_Tendinopathy

The wealth of information in this article with diagrams was excellent in understanding this area of the body that gets so much daily use (abuse) in supporting our every move in getting around.
Although this area of my body is not causing any daily concern, it often just feels “heavy” and closely related to lower back pain on occasion. I’m grateful for these insights on causes and tips to prevent and provide relief when this “surprise” of daily maturing greets me some morning!
Thanks, Nancy, for sharing.
I am so glad you found this beneficial, Mary Jo. I believe that just the idea of using a knee pillow can help with many things that ail us. Plus, it’s just good posture that helps our body alignment. Best wishes and keep moving. Nancy